Getting some fresh air has long been viewed as an important part of staying in good health. (Shutterstock)
Julia M. Wright, Dalhousie University
The New Brunswick legislature recently passed a motion to improve indoor air quality in the province’s public buildings “to reduce the spread of airborne illnesses, such as COVID-19.”
There are many ways to improve the air we breathe indoors, including filtration and ventilation: bring fresh air in, send exhaled air and contaminants out. And we have good reasons for looking at indoor air quality.
From wildfire smoke, to industrial pollution, many of us have felt the impacts of poor air quality and turned to air filters and respirators to cope.
The White House held a summit last year on improving indoor air quality to reduce the transmission of COVID-19. This September, there will be a similar meeting in Europe organized by the World Health Organization.
How new is all this? Well, it is and it isn’t. Eighteenth-century physicians were big advocates for ventilation as a way of reducing the transmission of contagious diseases, though not entirely for sound reasons.
Ventilation and eighteenth-century medicine
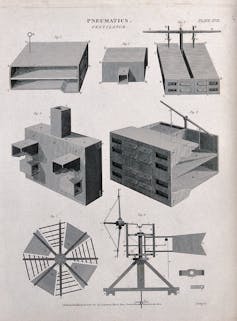
An 1817 engraving showing ventilators by W. Lowry. (Wellcome Collection)
I teach about eighteenth-century literature and medical writing in the British Isles. In the 1700s, British physicians took advantage of new scientific approaches but had little technology to see what was going on.
They believed that most contagious illnesses spread through smelly decaying matter, or miasma, from rotting food, sick bodies and so on. This is called “miasma theory,” and it was eventually replaced by germ theory.
Miasma theory meant that physicians associated bad smells with disease. But they also had the evidence of their eyes. Eighteenth-century physicians saw diseases spreading easily in crowded, poorly ventilated structures, from ships and jails to the homes of the poor. Ventilation made sense as a way to make people safer: blow out the bad air. It also seemed to make a difference when they used it.
So they acted. In 1756, the British Navy ordered the installation of recently invented ventilators on ships. A naval hospital required “doors and windows to be opened for the purposes of ventilation.” In 1802, the British parliament passed legislation requiring factories to have enough “Windows and Openings…to insure a proper Supply of Fresh Air.”
Outbreaks in the Navy
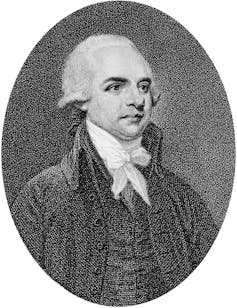
A 1796 engraving of Thomas Trotter by English artist Daniel Orme. (Wikimedia)
In his 1797 book on naval medicine, physician and poet Thomas Trotter drew on his extensive experience at sea. He questioned both miasma and germ theory.
However, Trotter partly agreed with miasma theory. He was convinced that many contagious diseases, including smallpox, were spread by “the exhalations of the sick.”
We now know that smallpox was spread via respiratory droplets or fine-particle aerosol. Trotter was basically right about the pathway for smallpox transmission — and a few other diseases — even though he was very wrong about how.
Eighteenth-century physicians had successes with the partial information they had. Trotter explains how they ended an outbreak of a “malignant fever” on a navy ship in 1791. They quarantined the sick, fumigated the vessel and “the ventilators worked unremittingly day and night.”
Ventilation spreads
These ideas spread widely beyond medical circles through literature and kept spreading after germ theory. Writers paid a lot of attention to “exhalations.” In his 1744 poem on health, John Armstrong wrote, “It is not air / That from a thousand lungs reeks back to thine.” Dozens of poets repeated phrases such as “infectious breath,” from Thomas Carew to Thomas Godfrey and more.
Like eighteenth-century doctors, nineteenth-century writers promoted ventilation and fresh air. In fiction, Jane Austen had her characters “breathing fresh air,” while Lady Morgan complained about “thickly populated and ill ventilated” streets helping to spread disease.
Some famous poets wrote about air so much that American literary critic M.H. Abrams remarked, “That the poetry of Coleridge, Wordsworth, Shelley, [and] Byron should be so thoroughly ventilated is itself noteworthy.”
From wildfire smoke to pollution, many of us have felt the impacts of poor air quality and turned to air filters and ventilation to cope. (Shutterstock)
Ventilation comes back
By the 1840s, the public health debate was turning to cleaner water, as germ theory began to take hold. But advances in germ theory couldn’t erase the benefits of breathing fresh air from the public consciousness. Around 1850, journalist Henry Mayhew interviewed one Londoner who said the following about the city’s cheap housing:
“Nothing can be worse to the health than these places, without ventilation, cleanliness, or decency, and with forty people’s breaths perhaps mingling together in one foul choking steam of stench.”
In 1859, Florence Nightingale helped revive ventilation in healthcare. In her book Notes on Nursing, she emphasized, “The air within as pure as the air without.”
Fresh air was seen as critical during the 1918-1920 influenza pandemic as well. People were encouraged to keep windows open and move events outdoors, including court proceedings.
Now, another pandemic has got us talking about the importance of fresh air. The difference is this time we have better tools to measure and improve indoor air quality, and a much better understanding of why fresh air is good for us.

Julia M. Wright, George Munro Chair in Literature and Rhetoric, Dalhousie University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
"Voices of the RSC” is a series of written interventions from Members and Officials of the Royal Society of Canada. The articles provide timely looks at matters of importance to Canadians, expressed by the emerging generation of Canada’s academic leadership. Opinions presented are those of the author(s), and do not necessarily reflect the views of the Royal Society of Canada.