WHAT WE KNOW – AND DON’T KNOW – ABOUT MASKS
Hedi Zhao, Sukhdeep Jatana and Mark Loeb | July 2, 2020
Hedi Zhao and Sukhdeep Jatana are medical students at McGill University. Mark Loeb is an infectious disease physician and professor of pathology and molecular medicine at McMaster University.
The debate over wearing a mask to prevent the spread of the coronavirus seems to be getting more emotional by the day. In the United States, proposals to make masks mandatory have led to intense arguments and speeches, as we saw at a Palm Beach County commissioners meeting in Florida last week. Tensions are set to rise in Canada, too, with places such as Mississauga, Toronto and Peel Region moving toward mandatory mask wearing in indoor public spaces. The act of donning a simple piece of fabric over the mouth has become a symbol of our new and dangerous reality – and an expression of people’s deeply held political views and beliefs.
In the absence of an effective therapy against COVID-19, and with a vaccine not yet on the horizon, non-pharmaceutical interventions such as the use of masks have taken on an added importance. All this warrants a look at the research on masks and their history to see what the evidence is for wearing them in the pandemic.
It was in 1897 that a mask was first used during surgery by French physician Paul Berger, who wanted to shield his patients from his saliva (he had a dental infection). A variant of this mask was used at an open-air hospital in Boston during the 1918 flu pandemic and led to speculation that a combination of masks, natural ventilation and strict hand hygiene reduced infection rates.
Over the course of the century, masks underwent continual evolution, from Berger’s rudimentary six strips of gauze to the development of the N95 mask in 1972 by 3M. Today, surgical masks are commonly worn by health care workers within the operating room to protect the sterile field. They are also used to protect health care workers from patients with suspected respiratory viral infection, typically worn upon entry to the patient’s room and for “source control” – that is, to protect immunosuppressed patients from health care workers who may be infected.
N95 respirators are worn to protect health care workers from patients who may have infections such as tuberculosis. Currently they are being used to protect against COVID-19 infection during high-risk procedures such as intubation (inserting breathing tubes) or bronchoscopy (when a thin tube is inserted into the airway to examine the lungs), which can generate aerosols.
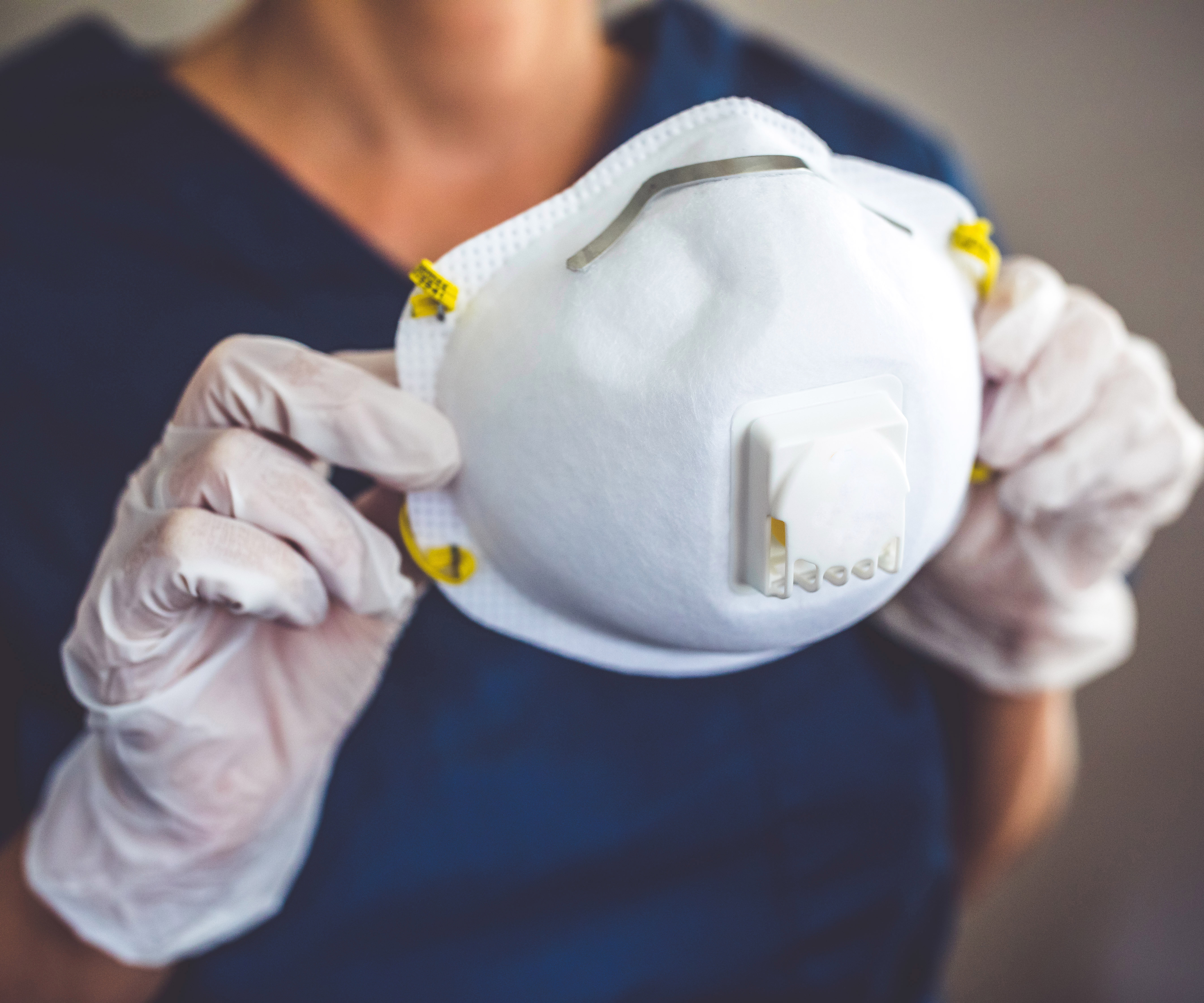
There is a stark difference between a surgical mask and a respirator such as the N95. A respirator prevents small airborne and larger droplet-borne infectious particles from entering. The name refers to the fact that the respirator blocks at least 95 per cent of small (0.3 micron) test particles. These devices are made of multiple layers of non-woven fabric, including outer protective layers, a prefiltration layer and a high-efficiency layer that determines filtration. The process for testing N95s is stringent and includes test conditions at a particular airflow, humidity and temperature, as well as the use of neutrally charged particles of the size most likely to pass through the mask. Users must also undergo a fit test to ensure a tight seal around the edges of the mask to prevent leakage, occasionally requiring different models for optimal protection. Individuals with stubble growth, a beard, a mustache or sideburns that cross the respirator sealing surface may fail this test.
Medical masks, also known as surgical masks, similarly undergo regulated testing, but often using less stringent standards, as they are intended to trap the wearer’s secretions and deal primarily with large droplets. When tested against the same standards as respirators, their filtration is highly variable depending on the model, ranging from 10 per cent to 90 per cent. Thus, medical masks are considered by the World Health Organization to sufficiently protect health care workers from patients with upper respiratory tract infections including the coronavirus during non-aerosol generating procedures. However, N95s should be used in higher-risk situations, such as interacting with patients who have infections transmitted via small airborne particles, as is the case with tuberculosis, or during procedures that generate these aerosols.
When putting on or taking off a mask in a medical setting, training is required. Prior to putting on a medical mask, individuals should first wash their hands. They should then cover their mouth and nose with the mask and make sure there are no gaps between their face and the mask. It is important to avoid touching the mask while wearing it. It should be removed from behind, without touching the front of the mask, then discarded. The hands should then be washed again.
The length of use of surgical masks and N95 respirators can be uncertain. Surgical masks are more frequently discarded because of their low cost and greater availability. Manufacturers of N95 respirators generally specify that they should be discarded if they become soiled or used during an aerosol-generating procedure. However, other than this, there is little guidance from the manufacturers or from public health authorities about how long these devices can be safely used. Sterilization and reuse of N95 respirators is currently under consideration at many Canadian institutions, but data about the safety of disinfection and reuse is limited.
It’s still uncertain how health care workers can best protect themselves in a clinical setting during the pandemic. There have been no randomized trials, the most rigorous form of evidence, comparing surgical masks to N95 respirators for COVID-19, although one study is being conducted in Canada. A pooled analysis of four controlled trials involving a total of 5,549 health care workers randomized to use either surgical masks or N95 respirators showed no significant difference in laboratory-confirmed respiratory viral infection between the two types of masks. While evidence with respect to COVID-19 is pending, it is widely agreed that wearing any mask offers more protection than wearing nothing at all.
The evidence for the use of masks in the community is even more controversial. In two community studies, investigators found no significant benefit to wearing a mask in everyday life interactions among family members with upper respiratory illnesses, although the sample sizes were small. Recent mathematical modelling, however, is suggestive of the benefit of universal mask wearing in the community when the uptake is at least 80 per cent. An evaluation of the characteristics of cotton masks and aerosol properties suggests they may lead to a possible modest benefit in the reduction of transmission, however no studies in populations for COVID-19 have been performed.
So where does this leave us? Current recommendations by public health organizations, such as the U.S. Centers for Disease Control and Prevention, advise cloth face coverings when around people outside one’s household, especially when it is difficult to maintain physical distancing, as this may offer a form of source control (that is, not protecting the user but rather others). The WHO advises the use of cloth masks in settings where there is widespread transmission, where the capacity for control measures is limited and especially in settings where physical distancing is not possible, such as on public transit or in stores. Given that cloth masks may help with source control – and wearing one causes little harm – this approach seems reasonable.
This article initially appeared in the Globe and Mail on July 1 2020.