
READING THE ENTRAILS: USING WASTEWATER EPIDEMIOLOGY TO TRACK COVID-19
Alex MacKenzie, Robert Delatolla and Doug Manuel | December 1, 2020
Alex MacKenzie, Robert Delatolla, Doug Manuel
Alex MacKenzie is a Professor of Pediatrics at University of Ottawa and Clinician Scientist at the Children's Hospital of Eastern Ontario.
Robert Delatolla is an Associate Professor in the Faculty of Engineering at the University of Ottawa.
Doug Manuel is a Senior Scientist at the Ottawa Hospital Research Institute.
We may be done with COVID but clearly COVID is not done with us. Even as we hear about promising vaccines and therapeutics, the current resurgence has us transfixed by a new epidemiologic stock market…local infections up, down, or holding? Alberta tracking up, Ottawa holding steady while PEI doing its best imitation of New Zealand. But how do you follow a virus beyond case counts, and hospital statistics? Since the 1960s, we’ve been able to measure human waste for traces of diseases like polio. The SARS CoV2 virus sheds from the intestine into stool from the first week of an infection and often for several weeks thereafter. And the sicker the patient, the more virus gets shed. And thus today, we have a new surveillance tool: Measuring the virus, or more precisely the CoV-2 RNA molecules – basically the genome of the virus that causes COVID-19 infection- in wastewater.
Our team from the University of Ottawa and Children’s Hospital of Eastern Ontario are measuring virus RNA levels in samples taken from the Robert O. Pickard Environmental Centre, the wastewater plan that serves close to a million people in Ottawa. Every day, samples taken over the previous 24 hours are relayed to University of Ottawa laboratories for testing for the CoV-2 RNA signature. The results are shared with Ottawa Public Health, as well as on the public 613covid.ca dashboard.
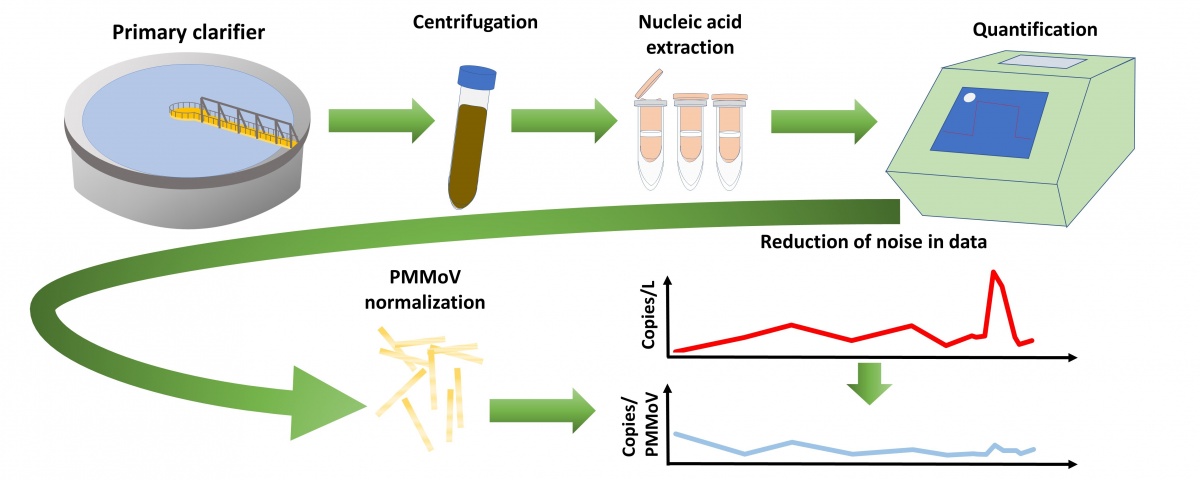
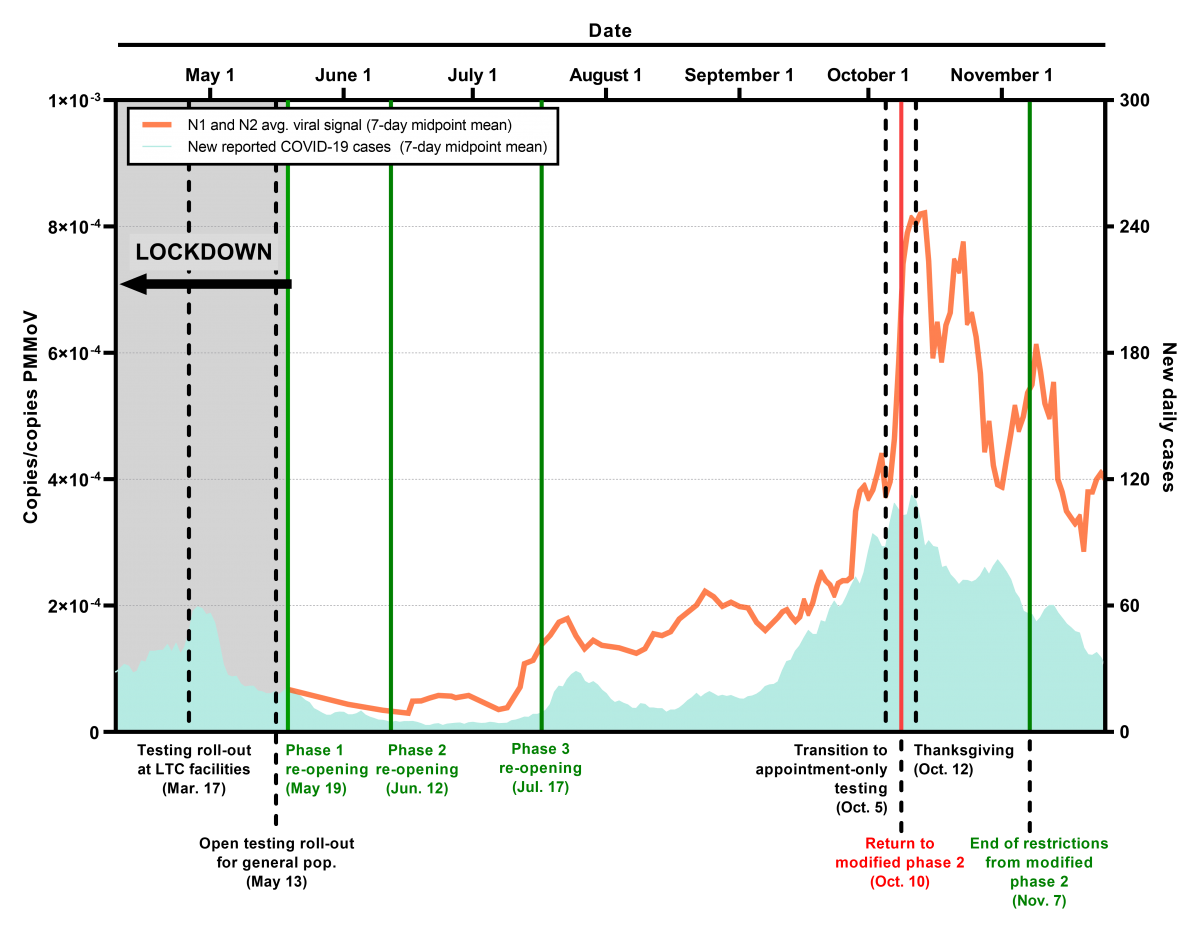
While there is a fair degree of variation in the data, as expected when measuring low levels of a fragile molecule in the harsh wastewater environment, it nonetheless serves as an important corroborating dataset for health authorities and the public, as we determine the level of community COVID activity. One of its chief virtues, besides a comparatively low cost, is the involuntary nature of enrollment; it is a survey to which we all contribute. Thus, while many persons with COVID have mild or no symptoms and don’t seek testing and others may not have access to testing, wastewater participation is an unchanging physiologic reality for all infected. It is not only data that generates reassurance for public health agencies and us all as we track COVID, it can also detect shifts in community viral prevalence. In mid-July, our wastewater readings identified a spike in Ottawa cases two days before increases in test positive cases and four before an uptick in hospitalisation level were observed (circled in figure). Thus, as a comparatively low cost, highly sensitive early warning system, it has enormous advantages. Whether a long-term care home, farm worker residence or correctional facility, the ability to rapidly identify an outbreak earlier than other methods will allow timely lockdowns, potentially obviate some of the expensive individual resident and staff testing while enabling the monitoring of outbreak trajectory.
In addition to measuring RNA, working with a Boston biotech firm, we have measured CoV-2 protein in wastewater detecting a much stronger virus signal. We are also beginning to look for antibodies against CoV-2, which are present in the stool of infected individuals as well as their blood. Our hope is that measuring of wastewater CoV-2 antibodies will be one means of gauging community or facility immunity. While our project is quite advanced, there are many other COVID wastewater epidemiology projects in Canada and globally. In an encouraging step, the Ontario government has recently committed funding to establish a regional sampling and testing network. The partnership of U of Ottawa and several other universities shall sample wastewater in locations across the province, providing results to local health units several times a week.
We’re still in a tough fight with COVID-19 infection rates still too high in Ontario and elsewhere. But, make no mistake, the deadly virus can run but it can’t hide and our tracking in wastewater will hopefully, hasten the day we can say we’ve finally defeated it.
This article initially appeared in the Globe and Mail on December 1, 2020.


