RACE AND ETHNICITY DATA COLLECTION DURING COVID-19 IN CANADA: IF YOU ARE NOT COUNTED YOU CANNOT COUNT ON THE PANDEMIC RESPONSE
Kwame McKenzie, CEO, Wellesley Institute | November 12, 2020
This paper discusses arguments for race and ethnicity data collection during COVID-19 and theories of how and why differences risk and the impacts of COVID-19 are related to race and ethnicity. It summarizes Canadian data on race ethnicity and COVID-19 before presenting ways to promote equity. There have been calls for race and ethnicity data collection to identify health disparities and promote heath equity in Canada for decades. They have not been heeded. COVID-19 has acted like a social x-ray, highlighting problems in our body politic. The higher rates and greater impacts of COVID-19 on racialized populations in Canada could be attributed, in part, to a lack of available data to identify inequities. But the fact that these data were not being collected; the fact that they still are not collected in most provinces; and, the fact the knowledge of disparities not has led to significant change in the pandemic response points to an underlying systemic resistance to pursuing health equity. Collecting race and ethnicity data, developing appropriate processes for governance and analysis, and ensuring that data is used for action are vital parts of a health system fit for Canada in the 21st century. But it will only happen if there is legislative change to deal with the systemic resistance to health equity for racialized people. It should not be legal to set up health care or pandemic strategies that predictably do not meet the needs of Canada’s diverse populations. It should not be legal to be deliberately blind to health disparities.
Canada is a multi-cultural country which claims diversity as a strength. There is social and cultural heterogeneity rarely seen in high income countries. And this has been used to develop a high standard of living. Canada consistently ranks as one of the best places to live in the world.
But this is not the case for all. There are significant socio-economic disparities and these lead to health disparities. Indigenous and racialized groups, particularly Canada’s Black populations, have an increased risk of a number of illnesses, poorer access to care and worse health outcomes. (1, 2)
The COVID-19 pandemic feeds on and exacerbates existing inequalities. Because of this, Canada’s social and health disparities have major implications for the development of evidence-based effective pandemic response. A one size fits all strategy is unlikely to work in a population with diverse needs.
Numbers have been vital in the fight against COVID-19. Countries have relied on the number of cases and the R- number to monitor the effectiveness of pandemic interventions and to decide when to move through lockdown phases. And the same numbers can be used to identify whether our interventions are working for everyone. To do this we need to collect socio-demographic data which can be disaggregated during analysis. If you are part of an aggregated sum you can be invisible in the numbers, your story will not be told, your needs will not drive policy action and your needs will not be met. In addition, disaggregated data are particularly vital in pandemics because the need for collective action. A response is as strong as its weakest link.
Good sociodemographic data and race based data are important tools for health equity but data collection it is not an end in itself, it has to be linked to action.
There are valid concerns about governance, accountability and protections against misuse of data. These issues need to be addressed because data is vital to the proper functioning of public health. Every doctor must take a history from their patient to ensure they make the right diagnosis and identify the most effective treatment. In public health, the patients are the population and the history is data. Public health needs good data to develop effective equitable interventions for communities and populations. We have already seen in Ontario that disaggregated data can save lives. Once Cancer Care Ontario were able to show that Black women were not being screened for cancers they were able to deploy one of the legion of evidence based strategies available to decrease disparities (3).
Collecting race and ethnicity data is now considered standard practice in health worldwide. Countries such as the UK and even our much-maligned neighbors to the south are able to report race and ethnic disparities in health. But Canada has lagged behind in the collection of these data. Race and ethnicity data is rarely routinely collected or reported at the Federal, Provincial or local level. This is despite evidence that it is feasible, there are Canadian evidence based tools to aid collection, there is a wealth of evidence that these data are useful in improving the quality of health systems in general and that they can be important specifically in pandemics. A study by Public Health Ontario during the H1N1 influenza pandemic reported that those who identified as South-East Asian were 3 times more likely to be infected, those who identified as South-Asian group were 6 times more likely to be infected and Ontario’s Black population was 10 times more likely to be infected (4). And, because Indigenous populations were at such high risk, the Ontario Government culturally adapted their public health response to try to improve outcomes.
Federal bodies such as Statistics Canada and health providers, planners and funders at all levels have resisted developing good race and ethnicity data streams. Because of this Canada went into the COVID-19 pandemic unable to identify or monitor crucial factors for the effectiveness and equity of our pandemic response.
During the response, they did not use the data they already had at an area level or attempt data linkages to try to understand whether there were race or ethnic differences in rates of COVID-19.
Later decisions to analyze existing data and collect race and ethnicity data during the COVID-19 response followed reports of clear race and ethnicity differences in illness rates from the USA and the UK, more acceptance of the concept of anti-Black and anti-Indigenous systemic racism in Canada and pressure from community organizations.
Manitoba was the first province to start collecting race and ethnicity data in its COVID-19 response (5).
Three public health units in Ontario; Peel, Middlesex-London and Toronto started collecting data between April and May 2020 and then the province of Ontario followed suit (6). Quebec initially said it would consider collecting race and ethnicity data for its COVID-19 response and then did not (7). Local Black entrepreneurs and community groups eventually launched their own website in and app in August 2020 to try to get data collected. They hoped this would spur their government to action (8).
By the end of the first wave the collection of race and ethnicity data in COVID-19 was not widespread. Most Federal COVID-19 linked programs were not collecting these data, and only 2 provinces were routinely collecting data. There were no adaptations of the public health or social pandemic response.
Why would race and ethnicity impact the rates of COVID-19 and the risks of harm?
Canada’s COVID-19 response has been good. In fact, our death rate of 23 per 100,000 is better than many other high-income countries. But it is worse than many others such as Germany (9)
One reason for this is that our initial response was focused on flattening the curve not who was under the curve. The focus on public health interventions for the whole population had some success but countries that were more successful added specific public health measures to protect at risk populations.
Long term care is perhaps the best example. CIHI has reported that 81% of first wave deaths in Canada were in long term care homes. Countries that had central control of long term care or developed clear early guidance for long term care at the time of their lockdowns did a better job at protecting this at-risk group and had much lower death rates. It has been calculated that at 4528 lives could have been saved if Canada’s first wave pandemic response was as good as Germany’s and much of that is because of their better performance in long-term care (10).
Focusing on who is under the curve as well as flattening the curve produces better outcomes.
Socio-demographic data is useful for understanding who is under the curve and once disparities in rates of infection have been identified, public health and social interventions can then be improved to ensure they equitably decrease risk. Subsequent data collection can monitor the effectiveness of interventions.
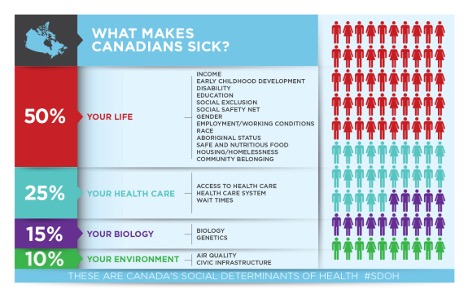
The Canadian Medical Association has calculated that 85 per cent of our risk of illness is linked to social determinants such as income, housing, education, systemic racism and access to healthcare. 15% is linked to biology (11). The COVID-19 pandemic adversely impacts health in four main ways:
- the disease itself;
- the public health response;
- changes in health services; and,
- the economic downturn. (5)
- Canadian Medical Association, 2013
These interact with the determinants of health so that the health outcomes are different for different parts of our population (12).
Impacts of the disease: COVID-19 impacts vary. Some have mild symptoms, some have severe symptoms, some make a speedy recovery and some have a more chronic illness with longer term impacts. The death rate is significant. The risk of COVID-19 and it impacts are influenced by the social determinants of health. Some populations such as racialized populations and Indigenous populations are more impacted than others by most of the social determinants of health. They have multiple, intersecting factors such as racism, poverty and social exclusion which work together to increase their vulnerability to illnesses. For instance, they are more likely to be essential workers and that puts them at risk and they are much more likely to work in long term care homes or hospitals. They are less well served by social and health services. (1, 2)
Biological factors such as Vitamin D have been offered as possible reasons for the high rates of COVID-19 in Black people in the UK and USA but the evidence is thin. It is based on the fact that the production of Vitamin D is dependent on sunlight and skin colour. People with darker living in the northern hemisphere are more likely to be Vitamin D deficient than others. Though appealing, this simple theory does not account for the high rates of COVID-19 in Black populations living in the sunny southern states of the USA. (13)
The more likely biological factors are actually the embodiment of social processes. For instance, racism has been shown to have significant impacts on health and risk of disease in part through hormonal changes and impaired functioning of the immune system (14). Obesity increases the risk of COVID-19 by up to 50% (15). Black populations in high income countries have higher rates of obesity and diabetes linked to poverty, low incomes, social inclusion and stress (1,2). Air pollution increases the risk and impacts of COVID-19 (16). Racialized populations in Canada are more likely to live in cities, (85% of the Black population of Canada lives in cities).
Impacts of the public health response: The public health response has an influence on the relative risk of infection. Those who can follow advice are more protected than those who cannot. Physical distancing and lockdowns also have direct impacts on physical and mental health. And, the inability to follow pandemic advice may increase mental health problems.
Those in congregate settings such as long- term care homes, the homeless and people in institutions find physical distancing difficult. But a bigger population is those living on the poverty line, in precarious work or in overcrowded homes. They are predictably less able to follow public health protocols and this puts them at increased risk of COVID-19.
And the harms of physical distancing and isolation such as stress, lower levels of exercise, substance misuse and domestic violence are more likely when people are overcrowded and when they have other social stressors such as workplaces that put them at risk or financial worries. Indigenous and racialized populations are more likely to be overcrowded, homeless or precariously housed than others.
Underlying the levels of stress linked to the public health and social response to COVID-19 is the concept of coherence and the factors that support health and wellbeing (17). In general people are happiest when they see that society has an understandable plan which could be effective, when they believe that the sacrifices they have to make for the plan are worth it and when they are given the support, tools and resources to make progress on societies plan. Canadian governments did a good job is getting people to agree to and believe in their pandemic plans but racialized, Indigenous and low-income groups are less likely to have the full resources to keep to the plan. Because of this they are at increased risk of COVID-19 stress related problems. The echo pandemic of mental health problems is likely to be patterned by these social determinants in COVID-19.
Impacts of changes in medical care: When hospitals and clinics moved into emergency mode, preventive medicine clinics shut down, outpatient visits and surgeries were cancelled, and some services moved to tele-health. Groups with existing health problems, those with existing access problems, those will less alternative health coverage and those without good digital access are likely to be hardest hit.
The economic downturn: The economic downturn will have direct impacts on health through stress, it may increase the risks of mental illness, suicide and substance misuse and it will also decrease access to care as health benefits are lost. Many of the social determinants of health such as housing and food security are linked to income.
Public Health England investigated race and COVID-19. They concluded:
“The literature review and stakeholder feedback indicate that risks associated with COVID-19 transmission, morbidity, and mortality can be exacerbated by the housing challenges faced by some members of BAME (Black and minority ethnic) groups. The most recent research from the UK suggests that both ethnicity and income inequality are independently associated with COVID-19 mortality. Individuals from BAME groups are more likely to work in occupations with a higher risk of COVID-19 exposure. They are more likely to use public transportation to travel to their essential work. Historic racism and poorer experiences of healthcare or at work may mean that individuals in BAME groups are less likely to seek care when needed or as NHS staff are less likely to speak up when they have concerns about Personal Protective Equipment (PPE) or risk.”
The situation in Canada for racialized, and especially Black and Indigenous populations seems no different.
Rate of COVID-19 for racial and ethnic groups in Canada
Data from the USA and UK reported that you were 2-3 times more likely to get COVID-19 and 2-3 times more likely to die if you are of African or Caribbean heritage. (18, 19, 20) These data coupled with community pressure led to studies in Canada. Because no individual level data was available initial analyses used the proportion of racialized groups in an area to try to get a handle on possible disparities.
Toronto Public Health reported that COVID-19 was more common in areas of the city with the highest Black populations (21) Public Health Ontario have found that infection rates are three times higher in areas where there were more racialized people. They also found that the mean age of infection was lower in these areas and the pandemic persisted in these areas when it had left other, (22). Quebec reported that more people died in Montreal Nord in the first wave of COVID-19 – a low income area with a high percentage of people of African and Caribbean heritage – than in the whole of British Columbia. In addition, the percentage of Black people living in a Montreal neighborhood was the strongest predictor of the rate of COVID-19 infection. (23)
As individual level data became available the scale of the disparities started to become clearer.
Middlesex-London Public Health Unit in Ontario report that 27 per cent of those who tested positive were visible minorities compared to 17 per cent of the population (24). Toronto Public Health figures showed that people who identified as Arab, Middle Eastern, West Asian, Latin American, South East Asian or Black were 6-9 times more likely to test positive for COVID-19 than the White populations (25). And, Peel Regional Public Health Unit published figures that showed South Asian, Black and Latin American origin residents were 40-100% over represented in COVID-19 cases and White residents were 40% under represented compared to their proportion of the population (26).
Differential harms of COVID-19 for racial and ethnic groups
The UK found that deaths from COVID-19 were increased by 2-fold in the Black and Minority Ethnic populations but all-cause mortality has increased by 4-fold (18).
A geographic study of COVID-19 in Ontario reported that hospitalization rates and admission to ICU for covid-19 are 4 times higher and death rates are doubled in areas with highest proportions of racialized people (22). Statistics Canada has recently released a crowdsourced survey which reports higher rates of generalized anxiety and poorer mental health of visible minorities compared to white people during COVID-19. (27). There is not good data on differential substance misuse, domestic violence or homelessness because of COVID-19 for racialized populations in Canada. There is evidence that before COVID-19 eviction applications were double in areas with high Black populations in Toronto indicating that this is a population at higher risk of homelessness (28). BC have undertaken a population based survey of the impacts of COVID-19.. “Caucasian” groups were less likely to avoid healthcare, had fewer impacts on their physical activity and they had fewer worries about their own health (29).
There are some data on the economic impacts. In a recent Statistics Canada crowdsourced survey 22% of white people reported that COVID-19 had moderate to severe impacts on their ability to meet financial obligations or essential needs. This compared to 44% of South Asian, 37.5% of Black and 36% of Filipino Canadians (27) According to the poverty institute of Canada there was an estimated 16 per cent job loss for visible minorities and recent immigrants because of COVID-19. Nearly 350,000 people in this group lost their jobs between Feb 2020 and May 2020. The total job loss for visible minorities is higher than low income workers and other groups such as indigenous people (30). BC’s population based survey of one in ten residents also reported significant differences in the social impacts of COVID-19. “Caucasian” groups did better than racialized groups. They had less difficulty making ends meet, fewer were not working and had less food insecurity. In addition, people with lower incomes (which is also more likely for racialized populations), were, less able to stay at home and work, were more likely to have a chronic illness, had more difficulty accessing healthcare and were less able to stay home from work when sick. Low income households reported more child stress (29).
What should we do with this knowledge?
The accumulated evidence supports the view that Canada has failed to properly and equitably protect its racialized populations from COVID-19. Racialized groups have increased risks of getting infected and increased medical and social impacts. In addition, our overall ability to flatten the curve and protect all Canadians is undermined by our inability to adequately protect our vulnerable populations. Canada relied on data from other countries for the problem to be highlighted and then communities had to push for data collection.
The lack of race and ethnicity data meant that we could not identify disparities in rates of illness. Our lack of data also meant we could not identify for whom our interventions were working poorly. We have been unable to see whether the pandemic strategies are closing or widening social differences, even though closing social differences may decrease COVID-19 risks. We have little data on the differential impact on children of racial and ethnic groups in COVID-19, but the worry is that stress and disparities in access to education will have health impacts.
Our inability to equitably protect racial and ethnic minority groups from COVID-19 is in part because data were not available, but also because the same systems that resist the collection and use of data undermine efforts to promote health equity. Seeing significant disparities and doing nothing active to deal with them is a form of systemic racism (31)
A health equity approach aims to decrease avoidable illness disparities between groups. It does this by ensuring that there is equal access to and outcomes from interventions. It takes a needs-based approach. When people or groups have similar needs the focus in on making sure they have similar access and interventions work equally well. (32)
If a group has greater need then the response increases and the interventions may change to ensure that their needs are met. Health equity would not mean that everybody gets the same COVID-19 response, but it should mean that the outcomes from the COVID-19 response are more similar. Evidence based tools such as health equity audit and health equity impact assessment tools have been used internationally and in Canada to promote health equity (32, 33). And, a variety of methods are available to improve equity by educating staff, adapting interventions and building better healthcare system access through the engagement and partnership with communities. There is no evidence that these strategies have been systematically deployed in the Canadian COVID-19 response.
A heath equity approach recognizes the risk of illness and the ability to recover are also linked to social factors. Changes to the social determinants of health to promote wellbeing of vulnerable populations are considered important health equity interventions (32). The fact that 85 per cent of illness risk is linked to social factors offers significant policy opportunities for improving health.
Health equity has a clear evidence base. But effective action may also need to understand the systemic barriers that stop best practice approaches such as data collection and evidence based health equity being deployed. We need to understand why previous pandemic research results were ignored. We need to understand why most provinces still do not think that data collection is required. And we need to understand why Ontario did not use the tool it developed to ensure health equity - (health equity impact assessment tool). We then need to develop legislative interventions to protect populations from systemic neglect (20).
Between mid-May and mid-July 2020 there were 3861 cases of COVID-19 in Toronto outside long term care homes. 83% of these were in racialized people and their rate of infection was at least 4.5 times that of the White population. If the rate in racialized groups was the same as the white group 2560 cases of COVID-19 would have been prevented. The numbers for Montreal, the epicenter of the Canadian pandemic, are not available.
It is unacceptable that Canada prides itself on its diversity and does not offer equitable protections for its diverse populations. However, the systemic nature of the resistance to the collection and use of race and ethnicity based data argues that we need legislative changes and central investment in the development of good quality socio-demographic data streams if we are to be able to identify at risk groups and produce, deploy, and monitor the progress of interventions. We urgently need data streams that will allow us to monitor the differential impacts of COVID-19. Data will need to measure health and social impacts. If race and ethnicity data were routinely collected by provinces and in the short form census it would help us to be able to use data we already collect to assess health disparities for COVID-19 and into the future. But accurate analysis of data for diverse communities requires capacity building so that both academic and community based researchers are able to be involved.
A better Canadian first wave COVID-19 pandemic strategy would have been based on an evidence informed and data driven, health equity approach. This should be the template for any subsequent waves and the recovery.
Recommendations
Four groups of actions are recommended to ensure that current and future responses to pandemics are equitable: Legislation; Equity based Pandemic Plans; Equity Based Social Policy and Recovery Plans; and, Improved Data and Research.
1) Legislation
We need strong legislation that ensures that our public health responses, our health response and our social policy responses produce as equitable outcomes as possible. Public services should promote race relations, they should produce equitable access to services and equitable outcomes of services and they should be required to collect data to prove that they are compliant.
2) Equity based COVID-19 health and public health plans
There need to be clear and published plans focused for promoting health equity in COVID-19 at each level of government. There also needs to be someone with the right seniority and resources who is tasked to ensure that plans are in place. The plans should use evidence based tools such as the health equity impact assessment, evidence based medicine techniques and community partnerships to adapt interventions as needed to ensure they are equally effective.
3) Equity based social policy and recovery plan
In addition to public health plans there needs to be a health equity lens taken to all associated Federal, Provincial and Territory responses to COVID-19. Taking a health equity lens to policies that impact the social determinants of health is necessary to facilitate a fairer response and to make sure that equity-based health and public health plans are not undermined by social policy that promotes inequality.
4) Data and research
COVID-19 socio-demographic and race and ethnicity data should be collected at all levels of government. Data collection, data analysis and subsequent actions should be undertaken in partnership with impacted communities.
Federal agencies such as CIHI and Statistics Canada should perform and publish COVID-19 analyses using existing sociodemographic information at the individual or area level.
Socio-demographic data including race and ethnicity data should be added to the short form census so that we have a full picture of Canada and a data set that can be linked to others such as health data to allow disaggregated analyses.
All Federal surveys should collect socio-demographic data including race and ethnicity data until such a time when linked census ethnicity data will be available. All Federal surveys should include sufficient people from the major racial and ethnic groups so that meaningful disaggregated and intersectional analyses can be undertaken.
The Federal Government should work with Provinces to produce good quality socio-demographic data including race and ethnicity for their health systems. One way of doing this is by facilitating the collection of race and ethnicity and other socio-demographic data at the time when people apply for and renew their provincial health insurance cards.
Federal research funding programs should include specific calls for work on COVID-19 socio-demographic inequities and race and ethnicity. These calls and programs may need to include funds for outreach and capacity building. Federal research funding programs should build a pipeline of researchers from doctoral students through to post docs and Canada chairs who focus on health equity and health disparities and in particular on the health of Black populations.
References
- Tracey Bushnik, Michael Tjepkema and Laurent Martel. Socioeconomic disparities in life and health expectancy among the household population in Canada 2020. Full article here
- PHAC Key Health Inequalities in Canada a National Portrait 2018 View here
- Engaging seldom of never screened women in cancer screening. A compendium of pan-Canadian best and promising practices 2010. View here
- Navaranjan D, Rosella LC, Kwong JC, Campitelli M, Crowcroft N. Ethnic disparities in acquiring 2009 pandemic H1N1 influenza: a case-control study. BMC Public Health. 2014;14:214. Published 2014 Mar 1. doi:10.1186/1471-2458-14-214
- Manitoba Charts New Course by Collecting Race Based Data on COVID-19
- Public Health Ontario - Introducing Race Income Household Size Language Data Collection
- Groups, advocates disappointed by Quebec's decision not to collect COVID-19 race data
- Quebec is still not publishing race-based data about COVID-19. These community groups aim to fill the void
- John’s Hopkins data accessed 25 June 2020 https://coronavirus.jhu.edu/map.html
- McKenzie K Lost lives analysis https://www.wellesleyinstitute.com/?s=lost+lives
- Canadian Medical Association,.. What makes us sick. https://www.cma.ca/health-care-canada-what-makes-us-sick
- We need data to protect those must vulnerable to the coronavirus
- Biesalski HK. Vitamin D deficiency and co-morbidities in COVID-19 patients – A fatal relationship?. Nfs Journal. 2020;20:10-21. doi:10.1016/j.nfs.2020.06.001
- Pascoe EA and Richman LS Perceived Racism and health a meta-analytic review Psychol Bull. 2009 Jul; 135(4): 531–554.
- Scheen AJ. Obésité et risque de COVID-19 sévère [Obesity and risk of severe COVID-19]. Rev Med Suisse. 2020;16(695):1115-1119.
- Martelletti L, et al. SN Compr Clin Med. 2020. PMID: 32296757
- https://en.wikipedia.org/wiki/Salutogenesis#cite_note-Antonovsky1990-5
- COVID-19: understanding the impact on BAME communities
- We need data to protect those must vulnerable to the coronavirus
- Anti-racism legislation needed to ensure equitable public health responses
- Personal communication from Toronto Public Health
- https://www.publichealthontario.ca/-/media/documents/ncov/epi/2020/06/covid-19-epi-diversity.pdf?la=en
- https://www.cbc.ca/news/canada/montreal/race-covid-19-montreal-data-census-1.5607123
- Personal communication of restricted Board minutes.
- https://www.toronto.ca/home/covid-19/covid-19-latest-city-of-toronto-news/covid-19-status-of-cases-in-toronto/
- https://www.peelregion.ca/coronavirus/_media/COVID-19-race-and-occupation.pdf
- Moser M, The mental health of populations groups designated as visible minorities in Canada during the COVID-19 pandemic https://www150.statcan.gc.ca/n1/pub/45-28-0001/2020001/article/00077-eng.htm
- Leon S and Ivenuik J Forced Out Evictions race and Poverty in Toronto https://www.wellesleyinstitute.com/publications/forced-out-evictions-race-and-poverty-in-toronto/
- https://www.cbc.ca/news/canada/british-columbia/covid-impact-racial-ethnic-backgrounds-1.5686051
- The Employment Impact of Covid-19 on Canada’s Equity Seeking Workforce
- McKenzie K, https://www.wellesleyinstitute.com/health/rethinking-the-definition-of-institutional-racism/
- https://www.wellesleyinstitute.com/topics/health-equity/
- http://www.health.gov.on.ca/en/pro/programs/heia/
- changes in health services; and, the economic downturn.